Английский язык. English in dentistry : учебник для студентов стоматологических факультетов медицинских вузов / Под ред. Л.Ю. Берзеговой. - 2009. - 272 с.
|
|
|
|
READING MATERIAL
Text 1. Read the text and answer the questions below.
OVERCOMING DENTAL ANXIETY
The Canadian Dental Association estimates that over three million Canadians suffer from dental anxiety. These are patients who continually cancel appointments, don't come in for check-ups and delay necessary treatment until they have a much more serious problem. The one million people who never see a dentist, the true dental phobics, are very likely to end up toothless!
With modern equipment and techniques, dentistry is now virtually painless. If you are fearful, the first step is to tell us - our goal is to provide you with the best dental care possible and we can't do that if you are not here! These are a few tips to help make your visit to our office worry-free.
Ask questions about procedures that cause you anxiety. If you know and understand what is going to happen, you will have less reason to worry.
- Eat a light meal before your visit and try not to drink coffee, tea or cola as they stimulate you instead of relaxing you. Eating a rich protein snack like a lean meat sandwich will help stabilise your blood sugar and reduce irritability.
- Distract yourself in the dental chair by using headphones to listen to the radio or to music you find relaxing. This will muffle noises that may bother you.
- Establish a signal, such as raising your hand, to let us know you want us to stop a procedure. It will make you feel more in control and give you a chance to ask for more anaesthetic if you feel any discomfort.
- The ways you deal with stress outside the dental office will work inside too! Try thinking of pleasant things, deep breathing or relaxing your muscles one by one.
- Some or all of these techniques may help you feel more at ease but, above all, don't be afraid to ask your doctor for a helping hand. That's what we are here for!
It's important that your child's dental experiences are as rosy and pleasant as possible. Frightened child patients grow up to be fearful adult patients, and that usually spells disaster for dental health. That is why, when all other means of relieving anxiety fail, we may recommend premedication. Certain mild drugs eliminate anxiety and fear. Parents should check out any possible allergies. Premedication is the last resort, but sometimes the best choice for putting a fearful mind at ease.
Vocabulary to the text:
to estimate оценивать
anxiety тревога, беспокойство, зд. страх, боязнь
to cancel отменять
virtually фактически
lean meat постное мясо
irritability раздражительность
to distract отвлекать
to muffle заглушать (звук)
to spell (disaster) означать, влечь за собой (бедствие)
at ease свободно, непринужденно
Questions to the text:
1. Why is it necessary to overcome dental anxiety?
2. What can be the first step?
3. What are the other steps which make a visit to a dentist worry-free?
4. Do you agree with them? Consider some other techniques which may help a patient feel more at ease in a dentist's office.
5. In what case can premedication be recommended? Why?
Text 2. Read and translate the text into Russian. Use a dictionary if necessary.
KIDS' TEETH: COMING OF AGE CAVITY FREE
Your children's cavity-counting days can soon be over. Pit and fissure sealants are a simple and effective way to stop the decay that causes cavities, especially in kids' teeth.
Here's how they work. Sealants are clear or white plastic coatings we can apply to the chewing surface of the back teeth. The sealant material covers the depressions and grooves on the surface of teeth where cavities are most likely to form. They work best protecting new teeth. That makes them ideal for children. Sealants give those teeth some protective armour through the ages of 7 to 15 when children are most vulnerable to tooth decay.
Depending on your child's chewing patterns, the sealants can last from six months to several years. We will check them at every appointment to make sure they are still doing their job properly. Sealants are not designed for areas between the back teeth or for front teeth. And teeth that already have fillings or decay cannot usually be sealed.
It takes only a few minutes to apply a sealant, and give your child's teeth years of insurance against decay. There is no drilling or freezing. This is a proven painless technique that can help preserve your child's smile for a lifetime.
Text 3. Read and translate the text into Russian. Use a dictionary if necessary.
PORCELAIN RESTORATIONS
THE PROPERTIES OF PORCELAIN
Porcelain has been used for the making of artificial teeth for such a long time that its properties are well known to all dentists. As prepared for dental purposes its colour and translucency can be made to simulate very closely the colour and translucency of natural teeth.
The hardness of porcelain is quite considerable; it varies in different specimens but is generally considered to be about equal to that of feldspar, which stands sixth in Moh's scale of hardness, diamond being in the tenth place and at the top of the scale.
The conductivity of porcelain for heat is low, as also is its coefficient of expansion, the latter being about the same as of platinum and half that of gold.
It is a very inert substance, being absolutely unaffected by any ordinary reagent, although it is rapidly attacked by hydrofluoric acid.
The material is supplied in the form of a fine powder, which when packed into required shape and fired to a proper temperature, is converted into porcelain with which we are all familiar.
QUALITIES OF PORCELAIN
From the description of the properties of porcelain already given, it would appear to be in many respects the ideal material for dental restorations, particularly in the front of the mouth. It has, however, certain limitations. As in the case of cast gold, the restoration has to be constructed outside the patient's mouth and then cemented into position in the tooth cavity, which must therefore be entirely free from all overhanging margins or undercuts. Thus in some situations when porcelain would be very desirable, it can only
be used if a considerable amount of sound tissue is sacrificed in the preparation of the cavity. This is particularly true in the case of interstitial cavities in anterior teeth (Black's Class III), which usually open proximally, and must be made to withdraw either lingually or labially if porcelain is to be used.
HYGIENE AND FREEDOM FROM HARMFUL EFFECTS
Porcelain is quite ideal in these respects, notably in the permanence of its glazed surface, in this respect contrasting markedly with the great majority of translucent cement fillings, which, as a rule, have a more or less rough surface.
The chief dental uses for porcelain are for:
• jacket crowns
• inlays
• additions to artificial teeth
PORCELAIN JACKET CROWNS
A porcelain jacket crown is a crown which is constructed so as to fit over the central portion of a tooth which has previously been reduced to a sort of cone.
The cases which usually call for this type of restoration are anterior teeth which are too hypoplastic or carious to be satisfactorily restored by fillings, but which still have sufficient dentine to make a strong cone. The appearance of malformed teeth such as peg-shaped laterals, and occasionally rotating teeth, may often be much improved by means of a jacket crown, though in the latter case the position of the pulp sometimes limits the desired change in form.
Occasionally, when a central incisor has been lost at an early age, the lateral may be moved into position and later built up in the form of a central, with very good results.
PREPARATION FOR VITAL TEETH
In making a preparation for a porcelain jacket crown, care must be taken to leave an adequate amount of dentine for the protection of the pulp.
If the tooth is in normal position, the enamel should be entirely removed. The shoulder around the neck of a tooth should be less than 1 mm in width, and only sufficient tissue above should be removed to free the preparation of undercuts and allow for an even thickness of porcelain. Further destruction endangers the pulp and does not add materially to the strength of the porcelain.
Another source of danger to the pulp is from heat produced by the friction of cutting. This will be entirely prevented if all cutting is done under a stream of cold water. Occasionally, cold water is also effective in overcoming pain, but more often local anaesthesia is required as well. It is better, however, to delay giving the injection until required, as the anaesthesia obtained will last through the later stages of the preparation when it is most necessary.
If the tooth is affected by caries, softened tissue should first be removed and replaced by zinc oxyphosphate cement. The preparation may then be made irrespective of existing caries.
PREPARATION FOR PULPLESS TEETH
It is sometimes desirable to make a jacket crown instead of a post crown in the case of a pulpless tooth. This is always worthwhile if a jacket crown is also required on one of the adjoining teeth, as the two crowns may then be matched exactly. It is sometimes also the best method when a crown is being made for a tooth which has had a root resection, as in these cases the root is not always long enough for an adequate post. A slightly shorter post will often be enough to strengthen the core or even to support an artificial core cast in gold. Whenever there is sufficient dentine left, the former method should be adopted, as an entire gold core tends to show through porcelain and spoils its appearance. This difficulty may, however, be overcome to some extent by the use of an opaque porcelain as the first layer in the building of the crown.
Text 4. Read and translate the text into Russian. Use a dictionary if necessary.
WHAT SHOULD BE DONE ABOUT WISDOM TEETH?
There are many good reasons for removing wisdom teeth also known as third molars, there are also some risks and complications that are possible when extracting these teeth and sometimes there are some good reasons for leaving them alone. The decision on a specific course of action must be determined by a well-informed doctor and patient working together.
• Consider first the many reasons that people choose to have their third molars extracted. The mouth is often too small for these teeth to fully erupt into a good functional position. This leads to one of several situations. The teeth remain completely buried in the bone of the upper and lower jaws
in which they developed, a condition known as impaction. In case of a
fully impacted tooth, it may continue to sit in the bone, surrounded by the
normal cyst in which all teeth develop. It may also happen that the normal cyst, later in life, enlarges and may even develop changes in the cells that line the cyst. When such cysts get large enough, they should be removed and examined by a pathologist.
• The teeth begin to erupt but are not able to assume their correct upright position. Most commonly the upper third molars will tend to face out towards the cheeks while the lower third molars will lean forward with just a small portion of the crown protruding through the gum. Teeth that are partially erupted lead to two problems.
First, they make hygiene of the second molars difficult leading to increased possibility of decay and gum disease (periodontal disease) around these important teeth. Second, the pink flap of gum tissue which partially covers the erupting tooth creates a warm, moist and dark pocket where bacteria which normally live in the mouth can use the food you eat to flourish, multiply and cause infection known as pericoronitis.
It is easy to understand why many people choose to have their wisdom teeth extracted while they are young and healthy and the teeth are surrounded only by a small normal development cyst rather than have to undergo a more extensive surgical procedure later in life when their recovery may not be as easy and their general state of health may not be as good.
Finally, some dentists subscribe to the theory that wisdom teeth may push the other teeth in the mouth forward and cause crowding and misalignment.
RISKS AND POTENTIAL COMPLICATIONS
Some risks and complications are common to all surgical procedures. These are infection, swelling, bleeding and the risk of anaesthetic itself.
And there are some risks/complications that are unique to the removal of third molars:
• The upper third molars have roots which often are separated from the maxillary sinuses by only a very thin layer of bone. Occasionally, a small communication is established between the sinus and the oral cavity when one of the upper third molars is removed. If this is the case, the normal procedure is for the area to be sutured and closed, appropriate antibiotics and decongestants to be prescribed, and the patient reappointed for follow-up. Most often this results in an uneventful healing period with no further treatment required. Occasionally, the area will heal open rather than closed, in which case an additional small surgical procedure will be required to close the communication.
• The lower third molars often have roots that lie very near or even wrapped around the inferior alveolar nerve. This is the nerve that supplies feeling to the lip, teeth and tongue on each side of the mouth. Occasionally, when a lower third molar is removed, that nerve will be bumped or bruised and, if so, a change in sensation may be noted on that side. It is important to understand that this is a sensory nerve and does not affect the ability to move the parts of the oral cavity to which it gives sensation (feeling). In most cases, the nerve heals itself but, because nerves heal slowly, it may take six months to one year before return of normal sensation. Very rarely, the damage to the nerve is permanent.
Text 5. Read and translate the text into Russian. Pay special attention to the questions and the answers given.
PERIODONTAL DISEASE
Periodontal disease affects 90 per cent of all adults and causes 70 per cent of all adult tooth loss. It is a pathological process affecting the periodontium, the tissue that invests and supports the teeth, the gingiva, cementum, periodontal ligament and alveolar and supporting bone. The disease results in inflammation of the supporting tissue of the teeth. This, in turn, results in a progressively destructive change leading to loss of bone and periodontal ligament. If the disease continues to progress without intervention, it results in compromised dentition.
What are the signs of periodontal disease?
1. Bleeding gums - your gum should never bleed.
2. Loose and migrating teeth.
3. Halitosis.
4. Swelling and abscess formation.
5. Recession of the gingiva.
6. Vague aching or itching of gums.
What are the treatment modalities?
Periodontal treatment is designed to eliminate the irritating factors, plaque and calculus. Ideal treatment consists of oral hygiene instruction, supraand subgingival scaling and antibiotic therapy. There is an abundance of evidence gathered over many years by numerous researchers that conventional periodontal treatment including surgery, combined with good microbial plaque control, is successful in arresting most cases of periodontal disease.
Today there is a growing debate regarding surgical versus non-surgical treatment of periodontal disease. Non-surgical periodontics involves a conservative approach toward treatment. Basically, it consists of all treatment modalities mentioned, without including surgery except in rare instances. In addition, a phase contrast microscope can be used to monitor the microbial environment.
What are the advantages of non-surgical periodontal therapy?
1) The obvious advantage of non-surgical periodontal treatment is that it doesn't require surgery and its attendant discomforts. And since fear is one of the prime deterrents to periodontal care, reduction in the possibility of pain can bring the benefit of care to larger groups.
2) There is less post-treatment root exposure, which reduces the possibility of temperature sensitivity and root caries.
3) Better aesthetic affects are achieved due to preservation of the gum tissue position as near the tooth crown as possible.
4) Some or all of this treatment may be performed by dental hygienists.
5) Bone tissue is not reduced in an attempt to create normal contour since the technique depends upon bacterial control regardless of tissue deformity.
What are the disadvantages of non-surgical therapy?
1) The dentist and periodontist have a greater responsibility to make an accurate diagnosis, explain their findings and treatment regimen, and discuss alternatives.
2) The patient's oral hygiene skills and motivation must be exceptional.
3) The technique is less predictable.
4) The maintenance interval and the instrumentation required at each interval become more critical. Patients on non-surgical maintenance care usually need more anaesthetic and more instrumentation.
What does the surgery involve?
Periodontal surgery involves elevating the entire soft tissue complex from the underlying alveolar bone by blunt dissection. The alveolar bone is exposed and made accessible for debridement and resection, thus promoting healthy generation. With the roots of the teeth exposed, the periodontist can remove plaque, calculus and stain from the previously unexposed tooth structure. The tissue is repositioned to the height of the alveolar bone and sutured. This eliminates the periodontal pocket which results in improved maintenance.
Text 6. Read and translate the text into Russian. Use a dictionary if necessary.
PERIODONTAL DISEASE IN CHILDREN
Although periodontal disease is more prevalent in adults, it's important for parents to realise that the disease affects all age groups. About 10 per cent of American children suffer from a virulent form of gum disease known as juvenile periodontitis. This rapidly advancing form of gum disease usually strikes the permanent teeth of otherwise healthy children. The disease often lacks symptoms, and the gums appear normal. Often, routine dental radiographs reveal bone loss around the teeth, and the disease is then diagnosed.
Some research indicates that a plaque-induced gum infection is responsible for the disease; others blame hormonal changes taking place during adolescence that may affect the body's immune system. Recent research suggests the disease may be hereditary and transmitted through the mother's genes.
When diagnosed early, juvenile periodontitis can be treated. If neglected, it can spread beyond the initially affected teeth to the remaining teeth and result in loss of permanent teeth.
Remember, check your teeth often for signs of gum disease. Practice good oral hygiene at home, and see your dentist regularly for professional cleansing and treatment. Early detection and treatment of periodontal disease can save time and spare painful, costly complications.
Text 7. Translate the text into Russian in written form using a dictionary.
FOOD'S EFFECT ON TEETH
If you are like many people, you probably eat more food than you really need, and the excess may take the form of sugar-rich between-meal snacks such as candy, coffee or tea sweetened with sugar, and sugar-laden soft drinks.
Foods containing starches may also cause tooth decay. Starch is present in cereals, bread, vegetables, fruits and processed foods. Researchers are not yet sure of the impact of starchy foods on the teeth. Some believe such foods are harmful if they are eaten frequently throughout the day; others believe they are not harmful unless they also contain sugar or are eaten with foods containing sugar.
The decay process begins with plaque - a sticky colourless layer of harmful bacteria constantly forming in the mouth. When you eat foods that
contain fermentable carbohydrates (sugars and starches) bacteria in plaque produce acids that can destroy tooth enamel. Each time acid is produced, it attacks the tooth enamel for about 20 minutes. After repeated acid attacks, the tooth enamel may break down and a cavity results.
When should I begin cleaning my child's teeth?
Even before teeth begin appearing, you should start cleaning the child's mouth to keep food residue and bacteria from damaging newly erupted teeth. After every feeding, wipe the baby's teeth and gums with a damp washcloth or a gauze pad to remove harmful plaque. You can sit on the sofa with the baby's head in your lap to make sure you can easily see the baby's mouth.
If plaque is allowed to build on the baby's teeth, the tooth enamel could become decayed. If the decay is left untreated, the primary teeth may be prematurely lost. Children need all 20 of their primary teeth for proper eating, speaking, and appearance. These teeth also reserve space in the jaw for the permanent teeth that later erupt. A complete set of healthy primary teeth allows proper development of a child's jaw and face. You should begin brushing and flossing your child's teeth after each meal or snack and before bedtime when all the primary teeth have erupted - usually when the child is between 2 and 3 years old. Ask your dentist to recommend a toothbrush for your child. Generally, a brush with soft, end-rounded or polished bristles is recommended because it's less likely to injure the gums. Children often need smaller brushes than those designed for adults. Toothbrushes should be replaced when bristles become bent or frayed, usually every 3 to 4 months. Pre-schoolers often wear out toothbrushes quickly because they brush imperfectly and chew on the brush. Inspect your child's brush often; wornout bristles do not remove plaque effectively.
Keep your child's teeth clean from the start. If you notice any signs of decay in the primary teeth, see your dentist promptly.
Text 8. Read and translate the text into Russian.
DENTAL EDUCATION IN GREAT BRITAIN
Curricula and teaching plans of dental education in Great Britain are not uniform and are arranged independently at each university, but in practice they are fairly similar since they are guided by the common recommendations of the General Dental Council.
The allocation of the dental course by departments in different universities is not identical. As a rule, there are the following departments: conservative
treatment of the teeth (including fixed prostheses), sometimes endodontic departments (treatment of pulpitis and pericementitis), periodontal (periodontal disease and diseases of oral mucosa); prosthetic (all kinds of removable prostheses); and pedodontic including orthodontics, as a rule. The latter is now and then an independent course but is more closely joined to the children's department and is not often linked with prosthetics. In some schools there is a prophylaxis department and an independent radiological department.
The organization of the teaching process varies in different schools. In some, there is a cyclical system when a student works in one clinic for some months, then goes on to another. In others, a parallel system is introduced when a student works the whole term or a year in several clinics.
At present great attention is paid (and correspondingly a great number of hours are spent in dental schools) to the teaching of children's dentistry. Gradually children's dentistry is becoming a leading discipline in the training of the dental student.
Fees for teaching are paid by students in all universities, in particular, for teaching at dental faculties. There are no government scholarships for students. A proportion of them receive grants from the county education department, and have to work off these grants on completion of their training. Some distinguished students receive university scholarships.
On completion of the training young specialists make their own arrangements for their work. A proportion of them, having received county grants, have to work off the grants received after the period of instruction. The majority start work as assistants to dental surgeons in general practice. Some manage to succeed in working up to an independent practice. To begin teaching or to take up a post of a scientific worker it is necessary to work for some years as a house surgeon and registrar in a hospital. It is necessary to spend a particularly long and many-staged training to be permitted to work in a surgical department of a hospital.
A school for dental auxiliaries was established in Great Britain only a decade ago. The length of training is two years. The first year consists of general preclinical training with elements of theory and work on the phantom head. Clinical training in the children's dental school takes place in the second year. On completion of their training the students are intended to be sent to dental surgeries of local children's schools, where they will work under the direction and supervision of a dental surgeon, carrying out, apart from procedures of hygiene (removing calculus, teaching the correct hygiene of the oral cavity), treatment of uncomplicated caries and extraction of deciduous teeth under local analgesia.
This type of an auxiliary is called a dental hygienist. The most important single aid to a dentist is an efficient chair assistant. The chair assistant should be able to help a dentist in all situations relating to operative procedure; therefore she should have the ability to identify and prepare materials, instruments and equipment for any routine dental procedures. Knowledge of sterilization, medication including anesthesia, tooth form and function, diet, nutrition, oral inflammation and first aid is important for the chairside assistant. It is also helpful for her to know roentgenographic techniques, office routines and supply management.
In general, the teaching in all dental schools is divided into two stages. The quantity of general medical subjects is considerably smaller than in the curriculum of Russian institutes (general pathology, bacteriology, general medicine and some other clinical disciplines). Special subjects such as anatomy and physiology of the oral cavity, pathology of teeth and oral cavity (including regional pathology and anatomy) and (in some schools) dental diagnosis are also included in the curriculum. The study of special clinical disciplines begins in the majority of schools with a rather extensive course in dental mechanics and study of dental materials, and a course of phantom head work in conservative dentistry from four to six months long. Great attention is paid to the technical training of a future dental surgeon.
Text 9. Read and translate the text into Russian and answer the questions that follow.
THE COLLEGE OF DENTISTRY OF NEW YORK UNIVERSITY
PART ONE
It is the third oldest and the largest private dental school in the United States. It is administered by the Kiser Dental Centre and is composed of clinics, laboratories, and other teaching facilities contained within several buildings. Since its foundation, New York University has been a private university, operating under a board of trustees and deriving its income from tuition, endowment (пожертвования ) grants from private foundations and government, alumni, corporations and other philantropic sources.
Being founded in 1865, the New York College of Dentistry became an integral part of New York University in 1925. With its prestigious background and contemporary perspective, the College of Dentistry, through significant contributions to dental education, research and patient care has extended its influence around the world.
A few years ago the College of Dentistry reached a decision to expand its previous three-year curriculum to a four-year curriculum. The curriculum is a synthesis of many areas of knowledge, including biology, physics, biochemistry, medicine, surgery, biomechanics, aesthetics, manual skills and social sciences. In addition to providing the student with a biological and social basis for application of clinical skills, the educational programme focuses on prevention as a much desired goal in dental practice and research. Advances in the dental sciences and the increasing dental health needs of the public call for an understanding of general health problems and greater cooperation with other health professions.
The educational goal is to educate and train clinically competent and sophisticated general practitioners, well-grounded in both basic and clinical sciences, fully prepared to adapt to changes in dental care needs and ready to keep up-to-date with the developing dental knowledge.
PART TWO
During the first and second years, the course includes both basic sciences and clinical sciences. Students receive instruction in principles of human behaviour, utilization of auxiliary personnel, practice management and other areas relating to the organization of work. They also have courses in nutrition, normal mastication, physical diagnosis and life support and cardiopulmonary resuscitation. Students are also required to choose one of the humanities electives. During the third year extensive didactic instruction is given in endodontics, fixed prosthodontics, occlusion, operative dentistry, oral and maxillofacial surgery, oral diagnosis, orthodontics, pedodontics, periodontics, radiology and removable prosthodontics. At the same time, special attention is being paid to instruction in general and oral medicine, detection and treatment of oral, and facial cancer, cariology. The fourth year is devoted essentially to the Comprehensive Care and Applied Practice Administration Programme which will orient the student preparing him/her for the practice of general dentistry and for providing comprehensive dental care in practice setting.
Clinical practice during the first and second years begins with a series of lectures on the dental patient aimed at preparing the student for the duties and responsibilities of everyday practice. The student learns the importance and the role of the dentist as part of the health team. During the second, and continuing into the third and fourth years, each student is assigned patients. Duties begin with examination of the patient and end only when
the patient's dental health is restored to the best possible state. The students are responsible for treatment planning, making appointments and providing dental treatment.
Research. While the College of Dentistry has long considered its primary mission is teaching, it has placed considerable emphasis on its research activities believing that an essential part of the education of dental students lies in the understanding of how research contributes to knowledge.
Requirements for Admission. All students applying to the New York University College of Dentistry must meet the minimum requirements as follows:
1. Completion of at least three years of study (a minimum 90 hours) in an accredited college or university.
2. The following minimum course requirements must be met: English - 6 semester hours' credit
Biology and physics - 6-8 semester hours' credit Inorganic chemistry - 8-12 semester hours' credit Organic chemistry - 6-8 semester hours' credit.
Additional courses in comparative anatomy, embryology, histology and electives are recommended. Courses fulfilling the above requirements are offered by the New York University's College of Arts and Science at Washington Square.
Notes:
alumni (plural from «alumnus») students бывшие студенты
electives зд .факультатив
Questions:
1. What is the oldest and largest dental school in the USA?
2. What is this dental school composed of?
3. Is New York University a state or private university?
4. What is the period of study at the College of Dentistry?
5. Do the students study social sciences there?
6. What does educational programme focus on?
7. What is the educational goal of this oldest dental school?
8. How is the idea of cooperation with other health professions reflected in the firstand second-year curricula?
9. In what way does the curriculum in the third year differ from those in the first and second years?
10. What is the aim in the fourth year?
11. When does clinical practice start? How does it begin?
12. When is a student assigned patients?
13. What are the student's duties in the course of clinical practice?
14. Who is responsible for treatment planning?
15. Why does the College place considerable emphasis on research?
Text. 10. Read and translate the text into Russian. Use a dictionary if necessary.
FORENSIC DENTISTRY
Forensic dentistry is an investigative aspect of dentistry that analyzes dental evidence for human identification. The forensic dentist plays an important role in our justice system. This field of dentistry is divided into forensic odontology and jurisprudence (the science of law). Forensic odontologists study and identify teeth, jaws, prostheses, dental appliances, bite marks, dental injuries, and dental records in the interest of justice.
Forensic dentistry is one of a number of forensic sciences. Other forensic sciences are listed below:
1. FORENSIC ANTHROPOLOGY examines and interprets skeletal evidence with methods used by archaeologists and with knowledge of human biological variation. This evidence includes bones, teeth, hair, clothing, artifacts, and scene analysis. The examination considers time of death, age, sex, race, body size and weight, individualization, and the cause and manner of death.
2. FORENSIC PATHOLOGY AND BIOLOGY utilizes autopsy, tissue study, and review of medical records in the investigation of injury or death as a result of accident, homicide, or suicide. Legal responsibility usually resides with a medical examiner or coroner. The criteria for death is irreversible cerebral function. The forensic pathologist attempts to determine and report on the (a) cause, (b) manner (homicide, suicide, accident, or unknown), and (c) mechanism of death.
3. CRIMINALISTICS includes fingerprints, ballistics, tool marks (chisel, hammer, etc.), and scene investigation to identify and analyze physical evidence in order to reconstruct the crime and to connect or eliminate suspects and victims.
4. TOXICOLOGY utilizes chemistry, photography, and biology to identify harmful substances within a body. These include medications, poisons, and illegal drugs.
5. FORENSIC PSYCHIATRY examines and testifies about the aspects of legal sanity, human motivation, and possible personality profile.
6. FORENSIC ENGINEERING uses engineers to investigate incidents such as airplane crashes, auto accidents, and structural collapse.
7. QUESTIONED DOCUMENTS TECHNICIANS study and report about printing, typewriting, handwriting, ink, paper, and other features of documents.
8. GENERAL FORENSICS involves other specialists who are qualified to analyze specific evidence such as designers, photographers, and technical experts. They might report, for example, in a case of product liability associated with death or injury.
9. FORENSIC JURISPRUDENCE involves criminal and civil lawyers using the earlier described specialists, reports, and testimony to pursue their case in our system of justice.
Notes:
forensic dentistry судебная стоматология
homicide убийство
suicide самоубийство; суицид
coroner следователь, производящий дознания в случаях
насильственной или скоропостижной смерти.
Text. 11. Translate the text into Russian in written form using a dictionary.
DENTISTRY AND HUMAN IDENTIFICATION
Dentistry often has much to offer in identification because teeth are the most durable parts of the body and dentitions are as individual as fingerprints. Situations involving decompositions and skeletal remains will yield no recognizable facial features or fingerprints. Postmortem (after death) teeth, jaws, prostheses, and appliances can yield a positive identification, given antemortem (before death) records.
Erroneous suspected identifications are often eliminated. The benefits of this are such that even with the lack of antemortem records, the effort is worthwhile to aid investigators with information from dental aging, sexing, and estimated socioeconomic grouping derived from restorative materials, attrition patterns, periodontal status, eruption patterns, skeletal features, and serology.
Forensic dental techniques most commonly include collection and preservation of dental and jaw remains, dental radiology, photography, impressions and casts, antemortem and postmortem charting, and the comparison of these records. Features are referred to as Points of Comparison and include (a) the number and identity of teeth, (b) tooth rotation, spacing, and malposition, (c) anomalies, (d) restorations and prostheses or appliances, (e) caries, (f) endodontic treatment, (g) implants
and surgical repairs, (h) pathology, (i) bone patterns, and (j) occlusion, erosion, and attrition.
DNA can be recovered from periodontal and pulpal tissues, and although DNA analysis has become an important tool in the forensic science armamentaria, it too has limitations including, but not limited to, time and cost. Forensic Dentistry techniques retain a valuable place in the scope of forensic sciences.
A well-organized approach results in accurate comparisons and minimizes the chance of error. The examiner should record each feature of the postmortem teeth and jaws and the radiographs on a standardized dental chart. The forensic dentist must carefully organize all evidence so that it is analyzed in a systematic manner using consistent and standardized methods.
Notes:
durable прочный, крепкий
DNA (deoxyribonucleic acid) дезоксирибонуклеиновая кислота, ДНК armamentaria оборудование лаборатории; оснащение
врачебного кабинета (включая инструментарий, аппаратуру и т.п.)
Text 12. Read and translate the text into Russian. Use a dictionary if necessary.
BITE MARKS
Numerous homicides and attack cases have been solved by bite mark identification, analysis, and comparison. Many bites are severe and leave telltale marks long after an assault. Dental casts and photographs from the suspect are made after obtaining a court-ordered search warrant. These techniques can be useful in solving some child abuse cases in addition to many assaults and homicides.
New technologies are coming to use in bite mark analysis to recover saliva DNA, digitalize photographic images, and preserve the unalterable original image on computers. Details may be highlighted to better see patterns but without physical change to the image. This method has withstood «chain of evidence» requirements. In the past, bite mark analysis had the vulnerability of some subjectivity and the inability to numerically quantify certainties. Today, when DNA can be collected, amplified, and analyzed with the standard accepted modern methods, it is possible to quantify the numerical probability of the association between the biter and the bite mark injury.
The forensic dentist must first establish the mark as a human bite mark, then identify, if possible, the teeth involved in the mark. Possibilities may involve missing, extruded, hypoerupted, rotated, tilted, chipped, and anomalous teeth. The dental forensic examiner must also consider the possibility of animal bites, victim self-bites, and marks from foreign objects that might be mistaken for a bite mark. Separate analysis of those markings may be useful to law enforcement agencies by connecting the victim's injuries to a tool or instrument owned by a suspect.
Law enforcement agencies are becoming increasingly aware of potential identifications from the dental profession.
The notorious mass murderer Ted Bundy (executed January 1989) was positively identified as the responsible person by his bite marks found on the buttocks of one of his young female victims. John Wayne Gacy of Chicago, convicted of 33 counts of murder, became a real test of the vital role forensic dentistry plays in the identification of the involved victims. Only five of the human remains found still had soft tissue, making the identification process a challenge. However, 20 of the 33 known victims were identified through their dental records.
Notes:
abuse жестокое обращение
assault нападение
search warrant ордер на обыск
enforcement agency организация по обеспечению правопорядка
notorious печально известный
Text 13. Read and translate the text into Russion using a dictionary and be ready to summerize it.
MASS DISASTERS
Forensic dentists have made many contributions to the identification of bodies involved in air crashes, mass homicides, structural collapses, floods, and similar disasters. The large volume of specimens and records demands a team approach with excellent organization.
The dental team is best organized into antemortem and postmortem teams of two examiners per team. One person handles the specimen and examines the radiographs, while the other person charts findings. The examining pair then reverses roles and checks each other's efforts. Antemortem charting and records must be done separately and stored separately from postmortem evidence during the investigation. An air crash investigation,
for example, can result in dozens to hundreds of records and take days to weeks to complete. Long hours of work are involved, as authorities and families seek answers and identifications quickly. There must be organization to avoid errors and oversights from fatigue and to provide the numbers of team members required to complete a project.
In mass disasters and in single human identifications, success at the task goes to the undaunted and determined examiner. Knowledge of dental anatomy is a basic. Dental forensic examiners also use close-up photography systems.
One particular disaster highlights vividly the unique skills and tremendous value of a forensic dental team in the accurate identification of bodies. Few can ever forget the horror that occurred at 8:30 p.m., 17th July 1996 off East Moriches, New York: the explosion of a 747 airplane, TWA flight 800 bound for Paris, France, with 230 passengers aboard. Within the first 12 hours, a team of 30 dentists, began the painstaking work of identifying the recovered bodies, which were devoid of clothing. Two and a half weeks later, 208 of the 210 recovered bodies and body parts had been positively identified. Identification of 95 was by dental records alone, another 60 by dental records along with medical records (radiographs, MRIs, etc.), medical anomalies, fingerprints, etc.
For the first time ever, all relatives were screened for DNA samples to compare with the more than 400 recovered body parts, enabling the return of each to the families for an appropriate resting place. Nuclear DNA samples were extracted from both bone and dental pulps, which was all that remained after the first week. Mitochondrial DNA was also extracted from ground tooth structure, but it is only effective in matching females.
One victim was identified by examining DNA on toothbrushes in his home. During toothbrushing, microscopic bits of tissue from the gums and mucosa are scrubbed off. In all, seven people were identified by DNA alone because no other method was available.
Altogether, 61 dentists and 22 auxiliary dental personnel participated in this important forensic project.
Summarise the text «Mass Disasters» using the following words and introductory phrases:
the text deals with..., it is said that..., according to the text..., forensic dentist, identification of bodies, disaster, mass homicides, dental team, dental and medical records, summing it up., in conclusion I'd like to say that..
Text 14. Read and translate the text into Russian. Use a dictionary if necessary.
COMPOSITE RESINS
There are several groups of composite resin materials; although most are tooth-coloured, some have been designed for use in anterior teeth, where appearance is most important, while others have been designed for posterior teeth where strength and abrasion resistance are of prime importance. In both cases the material is capable of being attached physically to the enamel by means of the acid-etch technique. Composite is strong in thin section when attached to enamel and so the enamel margins can be bevelled.
Composite resins can be attached to dentine by chemical bonding materials or via an intermediate layer of glass ionomer cement. Unfortunately, the bond to dentine is not as strong as the bond to enamel. Since the material shrinks as it sets, there is a danger that it will move away from the dentine towards the enamel in cavities bounded by enamel on one side and dentine on the other, as commonly occurs with cervical cavities.
All composites are a mixture of a resin and a filler. Fillers include quartz, fused silicon, and various types of glass including aluminosilicates and borosilicates. Some contain barium oxide to make the material radiopaque. Radiopaque materials must always be chosen for posterior teeth so that the material can be distinguished from dental caries on radiographs.
Conventional composites contain 60-80 per cent by weight of quartz or glass particles of sizes ranging from 1 to 50 mm.
Particle-size distribution may vary from one composite to another. The more modern materials contain larger quantities of smaller particles, making the material easier to smooth and polish.
Notes:
composite resins композиционные (зубопротезные) пластмассы
capable способный
etch травить, вытравливать
acid-etch technique методика травления кислотой
bevel снимать фаску, скашивать
bond связывать; связь, соединение
quartz кварц
conventional обычный
Answer the following questions to the text:
1. What is a composite?
2. What is the difference between various groups of composite resins?
3. How can composite resins be attached to dentine?
4. What do conventional composites contain?
Text 15. Translate the text into Russian in written form using a dictionary.
ALLOYS
PART ONE.
Glass ionomer cements
Glass ionomer cement is the most recently developed restorative material in general use. It adheres chemically to enamel and dentine. The bond to enamel is stronger than the bond to dentine because enamel is more highly mineralized. However, the chemical bond of glass ionomer to enamel is not as strong as the physical bond of composite to acid-etched enamel.
Glass ionomer cements are water based. They are routinely used with conditioning agents (a 10-second application of 10 per cent polyacrylic acid) to remove part of the smear layer. This is important to achieve the optimum adhesive bond.
'Cermet' is a version of glass ionomer cement which contains silver powder. Since the silver particles destroy the tooth-like appearance of the material, it is only used in posterior teeth.
PART TWO.
Cast gold and other alloys
The advantage of cast metal is that it is strong in thin sections and can be used to protect weakened tooth structure. This property is the major reason for using cast metal restorations, and cavities are designed so that weakened cusps are protected by a layer of metal. The cavity is prepared in such a way that the restoration (an inlay) is made outside the mouth and then cemented into the cavity.
At one time the small gold inlay was a popular restoration and innumerable inlays have served well for many decades. However, they cannot now be regarded as cost-effective by comparison with improved amalgam and other restorative materials and so are seldom made by most dentists. Therefore, the cavity design for small gold inlays is of only limited practical importance, but inlays still have a role to play for larger restorations protecting the tooth.
Notes:
glass ionomer cement стеклоиономерный цемент
smear зд. липкое вещество
cast gold and other alloys литьё из золота и других сплавов
cusp острый край зуба, жевательный бугорок
Answer the following questions to the text:
1. What restorative material is in general use?
2. Why is the bond to enamel stonger than the bond to dentine?
3. What is «Cermet»?
4. Why is «Cermet» used only in the posterior teeth?
5. What cast is used to protect weakened tooth structure?
6. Why are small gold inlays seldom made by dentists?
Text 16. Read and translate parts 1 and 2 of the text given below into Russian and answer the questions that follow them.
TREATMENT OF APPROXIMAL CARIES, TRAUMA, DEVELOPMENTAL DISORDERS,
AND DISCOLORATION IN ANTERIOR TEETH
PART ONE
Conditions affecting anterior teeth which may need restorations
The conditions affecting anterior teeth are as follows:
• smooth surface caries
• approximal caries
• trauma
• developmental disorders
• discoloured teeth
• tooth wear.
Approximal caries
Enamel caries starts on the approximal surface of anterior teeth just gingival to the contact area. It is less common than pit and fissure caries in the approximal surfaces of posterior teeth. This is because the anterior teeth are more likely to occur when the teeth are crowded and overlapping, because this increases the difficulty in cleaning between them.
It is difficult to diagnose early enamel caries at the white spot lesion stage, and so when a patient presents with established caries into dentine in one or more anterior teeth it is possible that the other contact areas have early enamel lesions. For this reason preventive treatment is important, including suitable dietary advice, the use of fluoride supplements (toothpaste, rinses, varnishes) and teaching the patient to use dental floss interproximally.
Dentine caries can usually be seen by transilluminating the tooth, either with light reflected from the mouth mirror or by a fibre-optic light. Transillumination is more effective with anterior than posterior teeth because they are thinner. If dentine caries is visible, then it is usually too late for a «prevent and observe» approach; a restoration is needed.
Approximal caries which also involves the incisal edge
A neglected carious lesion, or secondary caries around an approximal restoration, may undermine the enamel of the incisal edge to the point where the corner of the incisor breaks away under occlusal forces. Dentine caries balloons out in all directions from its approximal origin, and by the time that it undermines incisal enamel it is often close to, or already affecting, the pulp. The diagnosis of the caries is straightforward, but a vitality test and periapical radiograph are required to assess any pulpal involvement and/or spread of infection into the periapical tissues.
Trauma
Accidental damage to teeth has one of the following effects:
• fracture of the incisal edge involving enamel only
• fracture involving enamel and dentine
• fracture involving enamel, dentine, and pulp
• root fracture
• cracks in the crown of the tooth without loss of enamel
• no visible damage but damage to the pulp or its blood supply, leading in the long term to pulp necrosis
• partial or complete luxation of the tooth.
The restoration of enamel and dentine fractures will be dealt with here. A broken incisal corner involving the incisal edge and parts of the approximal surfaces is treated rather similarly to approximal caries which involves the incisal edge.
Developmental disorders
Previously, small areas of enamel hypoplasia were considered, and the treatment technique described involved preparation of the tooth and the insertion of a shallow restoration. In this article, larger areas of hypoplasia or discoloration are discussed. The techniques described are also suitable for other malformations including diminutive or peg-shaped teeth.
Discolored teeth
Several developmental disorders result in discolored teeth. However, a common cause of a single discolored tooth is pulp necrosis, where the break-
down products of hemoglobin discolor the dentine. A bleaching technique to improve the appearance of such teeth can be implemented in such cases.
Tooth wear
Tooth wear involving the incisal edges is also common. With modern diets, teeth do not wear appreciably at their approximal surfaces, although this did happen with primitive man.
Questions to part 1 of the text:
1. How are enamel and dentine carious lesions diagnosed?
2. What can you say about secondary caries?
3. What other conditions affecting anterior teeth are known to you?
PART TWO Treatment options
Composite resin materials came into general use in the late 1960s and early 1970s. This produced a revolution in the restoration of anterior teeth, allowing procedures to be undertaken, using the acid-etch retention technique, that were impossible with any previous material. Today, with the added versatility of light-curing materials many anterior teeth which would previously have been treated by crowns or extractions can be restored simply.
Uses and limitations of anterior composite materials
Provided that the occlusion is favorable, virtually the entire crown of an anterior tooth can be built up with composite, at least as a short-term restoration. This means that the majority of teeth with approximal caries, caries or trauma affecting the incisal edge, and many of the developmental disorders can be treated with composite alone. Tooth wear affecting the incisal edges is less successfully treated with composite since it tends to wear away quickly or break off. If it remains in place, its abrasiveness may increase the rate of wear of the natural opposing teeth.
Composite is limited in its use by the fact that it has a relatively low abrasion resistance, although composites vary in this respect, and also it sometimes becomes stained or develops a rough surface. Generally speaking, composites with a higher proportion of resin are prone to staining and those with a higher proportion of coarser particle size filler become rough as the surface wears down. These roof surfaces accumulate both plaque and extrinsic stain. If the occlusion is unfavorable, composite in contact with the opposing teeth will tend to break or lose retention.
Composite materials for anterior teeth are available in a variety of shades and in more opaque or more translucent versions. With large restorations it may well be necessary to use more than one shade to produce gradual colour changes across the surface of a tooth to match adjacent teeth.
Retention of composite to dentine
Anterior composite material should always be retained to the enamel by the acid-etch technique, even if the cavity is naturally undercut. This increases the marginal seal and reduces staining at the margins. However, composite is not retentive to dentine. In cavities, where the entire periphery is enamel, this does not matter because retention to enamel is sufficient, but in larger cavities where part of the border is apical to the cement-enamel junction and therefore has no enamel, retention to dentine is necessary. This is achieved in one of two ways:
• by an intermediate layer of glass ionomer cement
• by means of a dentine bonding agent.
The traditional method of retention is by means of retentive grooves and/or pins, and these have served for many years. Many dentists routinely used retentive grooves in dentine and a pin to support and retain composite replacing a broken incisal corner. However, even gold-plated pins may produce some discoloration in the composite, and their insertion carries some risk to the pulp. The use of glass ionomer cements or dentine bonding agents has now made these methods unnecessary.
Dentine bonding agents have been available for several years but are still being evaluated. Although the clinical results and laboratory tests for the early materials showed them to be effective in retaining composite to dentine surfaces, it became apparent that they were hydrolysing in the long term and reducing the durability of the bond. In addition, polymerization shrinkage of the composite may cause high stress at the bond.
Another problem with several of the dentine bonding systems which have been developed over the last few years (and in many cases these have disappeared from the market) was the complexity of the systems, with several bottles of liquid to be applied for different times. Many dentists found this too confusing and time-consuming to bother with. The newer dentine bonding agents are simpler to use, but do not yet have long-term clinical trial results to support their application. Yet another problem in using dentine bonding agents is that with large restorations it is necessary to use incremental packing, which is fiddly and time-consuming.
In contrast, glass ionomer cements are retentive to dentine, release fluoride, and have less polymerization contraction so that they can be used in
bulk to replace all the dentine, leaving space for one increment of composite to replace the enamel. Glass ionomer cements are now available both in their original auto-curing form and as resin-modified glass ionomer cements.
This is a developing field, and clinical research in the next few years is bound to influence clinical practice. At present, with large restorations where additional retention to dentine is needed for composite, the preferred approach is the glass ionomer cement-composite layered restoration.
Porcelain veneers
Porcelain veneers are cemented with composite resin to cover all or part of the labial surface of an anterior tooth. Porcelain has been used for crowns for over a century and is a very satisfactory restorative dental material in that it maintains its colour and surface gloss and is compatible with soft tissues.
Indications for porcelain veneers are where one or a number of anterior teeth are discolored or misshapen in such a way that it is necessary to cover the entire labial surface to disguise the problem and yet the other surfaces are sound. The advantage of porcelain over a composite veneer is that it is more durable in terms of colour and surface gloss, although it is more likely to fracture. The advantage of a porcelain veneer over a crown is that the tooth preparation is more conservative and also, because the palatal surfaces of upper incisor teeth are not prepared, the occlusion is not affected. However, some reduction of the labial surface is usually necessary and so the procedure is not reversible. The restorations are time-consuming and involve laboratory costs which are often as high per tooth as the cost of a crown. If the tooth being covered is very darkly stained, the thin veneer does not sufficiently disguise the colour and so it has to be made more opaque. For these reasons porcelain veneers have by no means replaced crowns and are unlikely to do so. However, they form a useful addition to the operative dentist's techniques.
Other materials and forms of treatment
The other two tooth-colored materials which have been used to restore anterior teeth in the past are silicate cement and acrylic resin (polymethyl methacrylate)). Neither of these materials is used now for permanent restorations, but many patients still have restorations in one or other of them. Silicate has the advantage of leaching fluoride and so is similar to glass ionomer cement in producing caries resistance. Its main disadvantages were its poor strength, so that it could not be used for incisal edge restorations, its poor solubility, so that the surface became progressively lost in many cases,
and its low pH before it set, so that careful precautions had to be taken to avoid pulpal damage.
Acrylic used as a direct filling material has a very high coefficient of thermal expansion and so expanded and contracted more than the adjacent tooth tissue, producing rapid marginal leakage. It did not prevent caries, and therefore secondary caries was common. It can readily be identified by its distinctive smell when it is cut in the mouth.
Questions to part 2 of the text:
1. What are the treatment options for anterior teeth problems?
2. Speak on advantages and drawbacks of using anterior composite materials.
3. What are the ways of retaining composite to the enamel today?
4. How do they compare with the traditional retention?
5. Why do dentists find it too confusing to apply dentine bonding agents and systems?
6. What is the preferred approach for large restorations today?
7. What are the indications for porcelain veneers? Why can't they replace crowns?
8. What are silicate cement and acrylic resin?
9. Why are they no longer in use?
I. TENSES
Exercise 1. Use Present Simple - Active or Passive:
1. A provisional denture (to use ) for a short period of time for reasons of esthetics, function, or occlusial support.
2. Most patients (not to prepare) to function without teeth, even for a short time.
3. The mouth (to contain) a number of different tissues, some of which, such as mucous membrane, connective tissue, blood vessels, nerves, muscle, and bone, (to find) throughout the body.
4. Foods (to differ) in their ability to stimulate salivary flow which, in turn, can influence their intra-oral effect.
5. The properties of an organism responsible for its pathogenicity (to call) virulence factors.
Exercise 2. Use Past Simple - Active or Passive:
1. The remaining teeth (to extract) and the fixed partial dentures (to remove).
2. Protein and vitamin levels (to exceed) the minimal recommended level.
3. Calculus deposits carefully (to remove ) from the selected teeth with a hand scaler.
4. The marginal fit of each crown (to examine) on the tooth.
5. A light-cured resin (to use) to fix each tooth.
Exercise 3. Use Future Simple - Active or Passive:
1. The odor of necrosis (to detect) usually even before the pulp chamber is opened because dentin becomes saturated with by-products of protein denaturation.
2. If caries is not managed preventively, the restorative treatment (to doom) to a cycle of disease, repair, new disease and further repair, and before too long, extraction.
3. Undermined enamel is brittle and in due course (to fracture) if subjected to occlusal forces, producing a large cavity.
4. The state of the tissue at any time (to depend) on the balance between the attacking forces and the defence reactions.
5. In many cases removing the adjacent tooth (to improve) access for cleaning, and even relatively large enamel lesions partially (to remineralize).
Exercise 4. Use Present Perfect - Active or Passive
1. Numerous analyses of the microbial make-up of plaque in subjects of different caries experience (to reveal) a correlation between the presence of Streptococci mutans and caries.
2. When an adjacent tooth (to extract) for other reasons, direct access is possible.
3. From the middle of the 17th century, gutta percha (to recommend) for all sorts of uses.
4. It (to use) in dentistry for over 130 years, as a temporary restorative, an impression material, or as a root canal filling material.
Exercise 5. Use Present Simple to denote future action:
1. If I still (to have) bad toothache, I (to see) my dentist tomorrow.
2. You (to develop) caries if you (to keep) taking sweets in such amounts.
3. When local treatment (to be completed), he (to be advised) what to do in future.
4. Only when the remaining teeth (to be extracted), we (to insert) an interim denture.
5. You (to avoid) psychological trauma associated with the loss of natural teeth if you (to agree) to use an interim denture.
II. MODAL VERBS AND THEIR EQUIVALENTS
Translate the following sentences into Russian paying attention to modal verbs:
1. The interim denture has to be physiologic and well tolerated by the patient.
2. Diagnostic casts are used to permit a topographic survey of the dental arch that is to be restored by means of a removable partial denture.
3. The tip of the gutta-percha point should extend to about 1-2 mm coronal to the apex during a try-in, because it will be forced further apically during condensation.
4. Government financial policy may also have an impact on dental practice.
5. The report concluded that oral health services and education of the personnel will need to be radically transformed.
6. It has to be recognized that some individuals with a high susceptibility to disease may be incapable of maintaining a natural dentition during their lifetime.
7. Prevention can be provided in the form of fissure sealant and topical fluoride applications to reduce future caries in these identified high risk groups.
8. When plaque is allowed to accumulate freely there is an acute exudative inflammatory response within 2-4 days in the connective tissue underlying the coronal portion of junctional epithelium.
III. INFINITIVE AND INFINITIVE CONSTRUCTIONS
Underline the infinitives and indicate their functions. Translate the sentences into Russian:
1. To be useful in predictive case-finding, a test must detect the majority of high risk children and, at the same, time identify those at low risk.
2. Clinically, the crevice depth is considered to be the distance to which a blunt probe will penetrate.
3. Rapidly progressing periodontitis is a term used to describe severe generalized periodontitis affecting young adults between 20 and 35 years of age.
4. Many different bacterial species are thought to be of aetiological significance in periodontitis.
5. The objective of oral hygiene education is to produce a change in behaviour which will result in a reduction of plaque accumulation sufficient, if possible, to prevent the initiation and progression of dental caries and periodontal disease, and to make the patient as independent as possible of professional support.
6. A large number of chemical agents have been tested for their ability to reduce plaque accumulation.
7. The UK data indicates not only that more elderly people are likely to have natural teeth in future, but also, that they are likely to have more of them than dentate people in previous generations.
8. If the operator is not confident that all the caries has been reached it is safer to remove the whole of the old restoration.
9. With increasing carious involvement of enamel and dentine, the area of chronic inflammation increases in size but it is believed to remain localized until pulp exposure.
10. Both white and brown spot lesions may have been present in the mouth for some years as it is not inevitable for a carious lesion to progress.
IV. PARTICIPLES AND PARTICIPLE CONSTRUCTIONS
Underline Participles and define their function. Translate the sentences into Russian:
1. The available material used today for root canal filling contains only about 20% gutta-percha, with the bulk being made up of compounds such as ZnO, silicates, etc.
2. In a slowly progressing carious lesion, toxins reaching the pulp may provoke chronic inflammation.
3. In chronic inflammation the cellular components predominate and there may be increased collagen production, leading to fibrosis but without immediately endangering the vitality of the tooth.
4. Such use of diagnostic casts permits a justification of the proposed fee through the patient's understanding of the problems involved and of the treatment needed.
5. The most common complication associated with a tooth being extracted is fracture of its roots.
6. The use of an interim denture may serve as a learning period for the patient.
7. Having decided on the abutments, the dentist is responsible for the preparation of the abutment teeth, for the design of cast restorations, and for the form of the occlusal rest seats.
8. Almost half the cost is concerned with restoring teeth attacked by dental caries.
9. Refined, finely ground and heat-treated starch can cause caries but the addition of sugar increases the cariogenicity of cooked starchy foods.
10. The tooth-attached plaque consists mainly of Gram-positive rods and cocci, while the unattached plaque consists predominantly of Gramnegative organisms including motile forms.
V. REPORTED SPEECH
Make the statements indirect paying attention to the use of tenses:
1. «About 2000 new cases of oral cancer occur in Britain each year,» said the reporter.
2. He said, «Much is already known about the prevention of dental caries and periodontal disease.»
3. The reporter said, «The possible influence of the hardness and calcium content of water on prevalence of dental caries has been suggested by many authors but investigated by only a few.»
4. «The main purpose of the study was to investigate how caries activity is influenced,» began the researcher.
5. «It has been suggested that all carbohydrate foods should be considered cariogenic,» said the scientist.
6. He concluded his speech with the words, «Less technical/manual skills will be needed, due in part to new technology, and more special skills in diagnosis, pathophysiology, disease risk assessment and management, and communication will be required.»
7. «Don't wait until caries develops,» the dentist said.
8. «Use small amounts of retraction force on the flap,» instructed the surgeon.
Turn direct questions into reported ones beginning with «Will you tell me»:
1. How should this information be used clinically?
2. How many years have you been investigating this phenomenon?
3. In what countries is fluoridated salt used?
4. Is arrested caries in distinct contrast to rampant caries?
5. When are fissure sealants applied?
6. What is the most common soft tissue injury?
7. May bacteria enter the pulp after exposure?
8. Why should caries develop in this way?
VI. WORD FORMATION
Exercise 1. The following prefixes are used to make words negative or with opposite meaning. Read and translate them into Russian:
a-, ab- normal abnormal
dis- appear disappear
il- legal illegal
im- possible impossible
in- visible invisible
ir- regular irregular
non- existent non-existant
mal- nutrition malnutrition
mis- understand misunderstand
un- known unknown
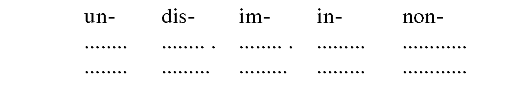
Exercise 2. Complete these columns by forming the negatives of each of the words listed below:
agree, accurate, able, certain, connect, employed, experienced, formal, like, likely, fortunately, honest, known, profit-making, readable, satisfied, stop, used, valid, natural, dependent, patient (adj.), important, order, cover.
 Exercise
3. Form words of the opposite meaning to those in column A, using one
of the negative prefixes, and fill in the blanks in the sentences.
Translate the sentences into Russian:
Exercise
3. Form words of the opposite meaning to those in column A, using one
of the negative prefixes, and fill in the blanks in the sentences.
Translate the sentences into Russian:
A B
1. appear The pain............ two days later.
2. visible X-ray examination helps the doctor to reveal inner disor-
ders...............to the eye.
3. valid They could not sell him the medicine at the pharmacy as
his prescription was............
4. connected Something is wrong with the lamp. It doesn,t work.
Oh, it's simply...............
5. likely Complications are very...............in this case
6. fortunately ..........the dentist could not see me, as I was half an
hour late.
7. usual Supernumerary teeth in the deciduous dentition are
very.........
8. agree His opinion was absolutely different, so he said that
he.. with the speaker.
9. order The dentist explained that such...............could be heredi-
tary or developmental.
10. smoker When we travel, we always choose the places
for.......
Печатные буквы | Прописные буквы | Название букв | Произношение |
А а В b C с D d Е е F f G g H h I i J j K k L l M m N n O o P p Q q R r S s T t U u V v W w X x Y y Z z | A a В b C c D d E e Ff Gg Hh I i Jj K k L l M m N n O o Pp Q q R r S s T t Uu Vv Ww Xx Yy Zz | ei bi: si: di: i: ef d3i: eitj ai d3ei Kei el em en au pi: kju: a: es ti: ju: vi: dablju: eks wai zed | [ei], [ae], [а:] перед г; [еэ] перед r + гласная [b] [s] перед е, i, у; [к] перед остальными буквами и в конце слов [d] (альвеолярный звук) [i:], [е]; [э:] перед г; [ю] перед г + гласная [f] [с!з] перед e, i, y (есть исключения), [g] перед a, o, u, согласными, в конце слов [h] [ai], [ι]; [э:] перед г, [aia] перед г + гласная [d ] [к] [l] (альвеолярный) [m] [n] [συ]; [о]; [σ:] перед г; перед г + гласная [p] [kw], редко [k] (пишется в сочетании с «u») [r] перед гласными; перед ^гласными и в конце слов не произносится [s], [z] [t] [ ju:], [л], [э:] перед r, [ jua] перед г + гласная [v] [w] [ks], [gz] в положении между гласными [ai], [ι], [э:] перед r, [as] перед г + гласная, [j] в начале слов [z] |